Inspection Day Turns Critical After A Child Swallows A Battery! | Learning Curve | Casualty
The waiting room clock ticked with a merciless rhythm as a storm brewed outside, its low thunder rattling the hallways of a crowded hospital. In this place where life’s fragile thread is tugged taut by every decision, a single misstep could unravel the entire tapestry. Behind the doors, doors that didn’t always stay shut against the soft murmur of anxious families and the sterile hum of machinery, a day of routine checks and badge-wearing formalities began to crumble into something far more perilous.
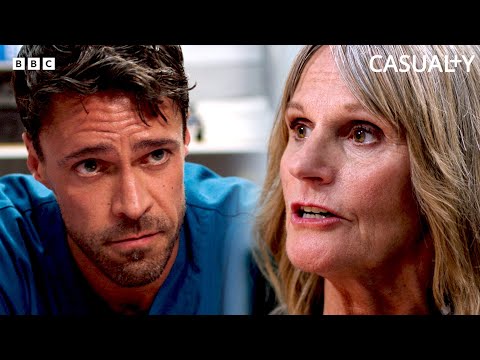
Dr. Flynn Byron stood in the corridor, a calm veneer over a restlessness that wouldn’t quit. He introduced himself with a practiced ease, as if to reassure both staff and patients that even in chaos there was order. Beside him, a younger face—Ceri Mayland from the regulator’s office—carried an edge of scrutiny that pierced through the hospital’s polished surface. The air between them crackled with the unspoken knowledge that a patient’s life can hinge on the slightest misstep, the smallest miscommunication.
A supervisor’s voice cut through the tension—Siobhan, a personification of consequence. This wasn’t a friendly tour or a ceremonial walk-through; it was a probe with teeth. The words came sharper than expected: not a box-ticking exercise, but a reckoning that could determine funding, status, even the very survival of the institution as a trusted teaching hospital. It pressed the team to face the possibility that the choices made in this moment would echo long after the inspection ended.
In the rooms where charts fluttered like wind-battered flags and the scent of antiseptic clung to every surface, a single crisis began to take shape. A child had swallowed a battery—the kind small enough to vanish in a moment and ferociously dangerous. The room erupted into a chorus of confusion and urgency. Questions—sharp, insistent questions—followed a frantic search for the culprit, the tiny culprit whose fate would demand immediate attention. Which child? Which battery? The search party moved with a frantic, almost desperate rhythm, praying the emergency would yield to skill and speed.
The team grappled with a collapsing plan. The radiology system—an essential lifeline in this crisis—had ground to a halt. The screen that should have lit up with images remained stubbornly dark, and the staff found themselves stranded at the edge of a widening chasm: the device that could save a life was out of reach, tethered to a fault in the hospital’s machinery. “Shall I take them to St James?” someone asked, the question a blunt, almost naïve hope in the face of imminent danger. But the response was a grim reminder of the real world’s constraints: time mattered, and every second counted.
With the radiology outage, improvisation became the new lifeline. The idea stored away in someone’s memory—metal detectors borrowed from security—emerged from the shadows, a makeshift beacon in the dark. The plan was audacious, risky: detect the elusive battery without delay, locate its hiding place in mouths or throats, and do it before the clock ran its cruel course. They scoured the ward for answers, for a sign of the battery’s location or absence, while the patient’s fate hung in the balance.
Yet even as they hunted for clues, the hospital’s systems hummed a warning: contingency plans, the solemn scripts of disaster drills, had never prepared them for a day like this. A full-scale inspection felt suddenly trivial beside the real drama unfolding in the ED. The team’s focus narrowed to a single goal: save the child who lay in resus, their lives a fragile balance between breath and blast of a devastating injury.
The child, Albie, drifted between moments of hope and danger. He had choked, his body’s own reflexes fighting a battle that could end with silence or mercy. The medical team moved as one, CPR becoming a steady heartbeat of the room, each compressive push a desperate prayer, each breath a whispered plea for revival. The lights, once just a question of function, flickered in the mind: would they hold? The room’s rhythm resembled a drumbeat, a pace that kept time with their frantic efforts and the mounting certainty that victory would demand not just skill but stubborn, unyielding will.
In the midst of the clinical storm, a human drama unfolded that cut deeper than any medical challenge. Ceri, the regulator’s observer, found herself pushed to the margins by the very people she was meant to assess. The room, with its alarms and murmured instructions, became a crucible where the truth of leadership was tested: not the appearance of competence, but the grit of accountability. They argued, not in anger, but in the sharp language of necessity—“Do you have a five minutes?”—a cruel reminder that in emergencies, time itself becomes the most elusive resource.
The hospital’s staff were pressed to improvise not only on medical grounds but on ethical ones: who could they hold as responsible if the battery’s path proved fatal? The weight of resignation loomed as a possibility to shoulder the blame. Dr. Byron, a figure of authority and responsibility, found himself confronting a future he could never truly predict. He spoke of handing in his resignation with a seriousness that felt almost poetic in its gravity: whatever it took, he would carry the consequences. The scene traded bravado for a sobering sense of duty—the knowledge that leadership sometimes means accepting the burden of failure when the system itself falters.
Outside the ED, a quiet exchange cracked the façade of clinical rigor. Hands off, hands on, the tension between privacy and urgency threaded through conversations about lines and oxygen and endoscopies. The team’s efforts to secure the airway in a room humming with monitors and the sound of medical equipment gave way to a more intimate moment: a bedside plea to protect a child’s life at all costs, even as the world seemed to push for a speedy resolution.
The narrative arcs toward a turning point that could redefine futures. A mentor’s assurance—an offer to be a shield against the storm—reveals the hospital’s humanity beneath the procedural armor. It’s a moment of risky courage: shielding colleagues from the consequences of a system that sometimes breathes failure, even as a plan is forged to salvage what remains of the day’s order. A few gestures of empathy break through the clinical dark—shared jokes, a taxi ride offered as a small mercy—reminding us that resilience often arrives as small kindnesses in a sea of fear.
As the night wears on, the tension doesn’t merely ease; it evolves. The team commits to a full inspection, a rigorous reckoning that will determine a future where patient safety isn’t just a protocol but a lived practice, daily and relentlessly. The clock may have narrowed the horizon, but the resolve expands, mapping a path through the shadows with the quiet stubbornness of people who refuse to surrender.
The labored breaths of Albie, the tremor of the room’s lights, the clack of keyboards and the whispered inquiries—these become a chorus. A life is at stake, and every heartbeat counts as a vote for what kind of hospital they want to be: one that answers the call in the hour of crisis with courage, competence, and a willingness to own the consequences, whatever they may be. In these moments, leadership isn’t a title but a practice—steady hands, clear eyes, and a plan that can withstand the most brutal tests.
And so, as the day borrows its last ounce of light from a stubborn sunset, the question remains for those who watched and worked: can they fix what’s broken, can they rebuild what’s frayed, and can they do so with integrity that outlasts the day’s fear? The outcome isn’t sealed in the patient’s fate alone; it rests with every decision made in the room—the choices that will shape not just this hospital’s future, but the trust the community places in it when the alarms finally quiet and the doors swing closed for the night.